Personalized medicine: treatment of acute stroke
If a blood clot in the brain blocks the oxygen supply, those affected suffer an acute stroke. Every minute counts when it comes to treatment. A team from Empa, Geneva University Hospital and the Hirslanden Clinic is currently developing a diagnostic procedure that will allow customized treatment to be initiated as quickly as possible, as they write in the journal "Scientific Reports".
One minute everything seems normal, the next the blood supply to entire areas of the brain is blocked: When a blood clot blocks a blood vessel, the oxygen supply to the nerve cells is interrupted and the affected person suffers an acute stroke. This life-threatening condition can manifest itself in many different ways: From muscle paralysis to loss of hearing or vision to unconsciousness. But one thing is always clear: this is a medical emergency and the time it takes to clear the vascular blockage must be as short as possible in order to save as many nerve cells as possible from dying. This is the only way to prevent permanent neurological damage.
It is not always easy to determine which treatment method is most suitable in such a hurry. Based on X-ray analysis and electron microscopy, a team from Empa, the University Hospital of Geneva and the Hirslanden Clinic is currently developing a method that should make it possible to determine the optimal therapy within a very short time. An initial study has now been published in the journal "Scientific Reports". This data should provide the basis for tailor-made treatment in the sense of personalized medicine.

X-ray each cell individually
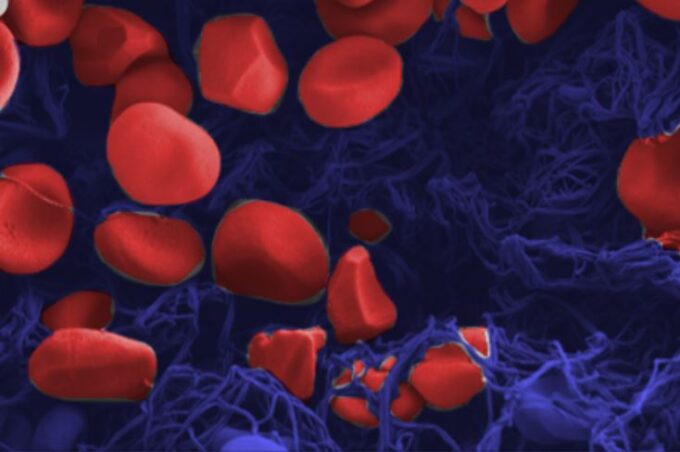
The reason: not all blood clots are the same; depending on the type, different cell types can clump together. Depending on whether red or white blood cells dominate or how high the proportion of protein-containing fibrin fibers is, the thrombus has completely different properties. In addition, the thrombi differ greatly in their shape. A 15 millimeter long thrombus that does not completely fill a blood vessel has different mechanical properties than a clot that is only a few millimeters long but completely blocks a vessel and paralyzes the blood supply to the areas of the brain behind it. The optimal treatment depends on these differences, whether it is dissolving the clot with medication or using a so-called stent retriever, a kind of tiny fishing rod with which the thrombus can be "fished out" of the blood vessel, and whose material can be selected differently depending on the thrombus.
In radiology, conventional computer tomography is currently used to make a therapeutic decision. However, the images of the patient's head hardly allow any conclusions to be drawn about the details of a clot, as objects made of similar material cannot be distinguished from one another or spatially resolved. In everyday clinical practice, we also have to make do with details that are limited to around 200 micrometers.
This is not the case with the laboratory methods used by the researchers in the new study: The team, including Robert Zboray, Antonia Neels and Somayeh Saghamanesh from Empa's "Center for X-Ray Analytics", examined various blood clots that had been removed from patients during neurosurgical procedures. Various laboratory technologies were combined for this purpose, resulting in virtual 3D findings with detailed and previously unknown properties of blood clots. "We used 3D micro-tomography to examine individual red blood cells down to the micrometer," says Empa researcher Zboray. Such tomographies with phase contrast methods produce a stronger contrast. Objects that are easy to penetrate, such as muscles, connective tissue or blood clots, can thus be depicted in particularly fine nuances and in their spatial distribution.
Calcified thrombi
Other technologies such as scanning electron microscopy and X-ray diffraction and X-ray scattering methods provided additional information down to atomic structures. Here it was shown for the first time that a thrombus not only consists of blood cells and fibrin threads, but can even be interspersed with minerals such as hydroxyapatite, as is known from vessel walls in arteriosclerosis.
However, this detailed information on the characteristics of a blood clot comes too late if the thrombus has already been surgically removed. In addition, the newly acquired data cannot be compared at first glance with the usual images and findings at the hospital. However, digitalization in medicine makes it possible to model the data in such a way that an algorithm could read out the detailed information in the future. "To do this, we need to examine significantly more thrombi so that we can use machine learning to recognize new characteristics and image patterns regarding the composition of the clots, which can then be transferred to hospital images and thus facilitate the identification of different types of thrombus," says Zboray.
According to the researchers' goal, conventional hospital images could then be interpreted in the shortest possible time as if the blood clot in the head had been examined in a virtual laboratory. Ultimately, this will allow stroke patients to receive more precise and personalized treatment more quickly.
Source: Empa